Japan Has Made Artificial Blood — Why It’s a Bigger Deal Than You Think
Japan’s synthetic blood is universal, shelf-stable, and may redefine emergency medicine by 2030. Here’s why it matters.


Imagine a world where every hospital, ambulance, and battlefield has instant access to safe, universal blood—no typing, no cold storage, no delay. That world is no longer science fiction. Thanks to a remarkable breakthrough by Japanese researchers, artificial blood may soon become a life-saving reality.
A universal solution to a global problem
Blood transfusions are critical in emergency medicine, surgeries, trauma care, and military applications. But they come with constraints: donors must be matched by blood type, stored at precise temperatures, and used within weeks.
Japan's synthetic blood project changes this narrative. The artificial blood is universally compatible, meaning it can be transfused into anyone—regardless of blood type. In high-stakes scenarios where time and compatibility are crucial, this innovation could save thousands of lives.
Moreover, this artificial blood is shelf-stable for up to two years at room temperature, unlike traditional blood which expires within 42 days and requires constant refrigeration. This makes it ideal for use in remote locations, disaster zones, and regions with limited infrastructure.
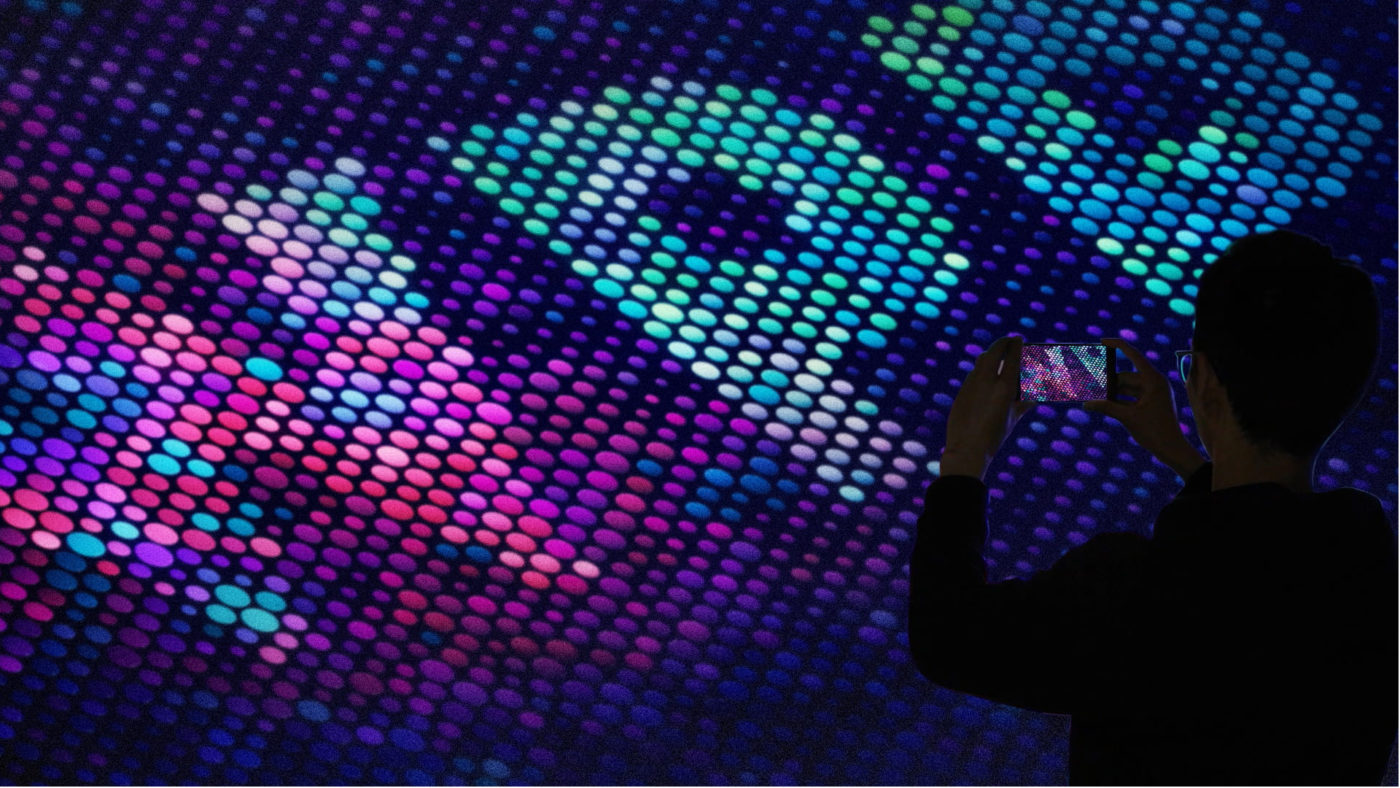
How it works: science in a bubble
Developed by researchers at Japan’s National Defense Medical College and other institutions, the artificial blood is created using a technique called hemoglobin vesicle (HbV) technology. Here’s how it works:
- Hemoglobin is extracted from expired donated blood.
- It is then encapsulated within synthetic lipid membranes to form nano-sized vesicles that mimic real red blood cells.
- These vesicles can carry oxygen through the bloodstream just like natural red cells.
- Some versions also include platelet substitutes, aiding in blood clotting—crucial during injuries or surgeries.
This combination allows the artificial blood to replicate two key functions of human blood: oxygen transport and coagulation.
Promising early trials, with eyes on 2030
Early trials have shown that small amounts of this artificial blood (around 100 ml) can be administered safely to animals and healthy human volunteers without serious side effects. In 2025, expanded human trials began, focusing on safety, absorption, and overall performance.
If clinical trials continue to show positive results, Japan aims for commercial approval and public rollout by 2030. Researchers believe the technology could play a crucial role in emergency medicine, military operations, and humanitarian crises around the world.
More than a medical breakthrough—it’s a global strategy
Japan’s innovation arrives at a critical time. The country has one of the world’s oldest populations, and its blood donor base is shrinking. As more nations experience demographic shifts and increasing demand for safe transfusions, artificial blood could help fill widening gaps.
Moreover, in crisis situations—natural disasters, terrorist attacks, war zones—relying on a steady supply of type-matched, refrigerated donor blood is a logistical nightmare. Artificial blood offers a portable, ready-to-use alternative that doesn’t compromise on safety or efficacy.
Challenges still ahead
Despite the enthusiasm, there are still hurdles to overcome:
- Scaling up production to meet national and global demand.
- Navigating complex regulatory approval processes.
- Ensuring the product remains affordable and accessible once commercialized.
- Testing efficacy in high-stress, real-world medical environments.
Other countries, including the US and UK, are also pursuing artificial blood solutions through various methods, from lab-grown red blood cells to freeze-dried hemoglobin powders. But Japan’s approach, with its stability and compatibility advantages, is seen as one of the most promising.
If successful, Japan’s artificial blood will revolutionize emergency healthcare, making blood shortages and compatibility issues a thing of the past. It’s not just a medical innovation—it’s a humanitarian tool with global implications.
As we edge closer to 2030, one thing is clear: the future of medicine may not run on donations, but on lab-engineered red.
Edited by Rahul Bansal