Why the big consulting firms are bad for healthcare
The healthcare industry has many ills. The payer-provider disconnect creates confusion, limits access, and exacerbates inefficiencies. Doctor and nurse burnout has led to widespread staffing shortages. This is compounded by aging infrastructure, outdated regulation, fragmented care delivery, and overly-complicated legacy systems. The list goes on. But there is a particular cancer that we could eliminate tomorrow: big consulting firms. Every year, American healthcare systems spend hundreds of millions of dollars on consulting firms that deliver PDFs instead of solutions. While patients suffer and clinicians burn out, these legacy firms collect their checks and move on—leaving implementation challenges to healthcare institutions they’ve diagnosed but failed to treat. Proponents of the “Big Five” consulting model would argue that sclerotic institutions need an untainted outsider to parachute in. Someone who isn’t married to the nuances of an existing system. But theorizing is easy to do when you’re not tethered to the results. In healthcare, it’s not just financial results the consultants are off the hook for, it’s people’s lives. What do providers get with a legacy consulting firm? Well, a sizable stack of documents. With massive fees to match. While a 300-page PDF may impress at first blush, it won’t lead to actionable, sustainable solutions. It certainly won’t allow the health system to rapidly test and refine new models of care delivery, proving which ideas do and don’t work in practice. Time pressure and fitting solutions in boxes At Cactus, the design firm I cofounded, one of our clients was let go from a major health system as part of a big consulting cost-cutting round. He had been working to reduce staffing shortages and developed a novel method for care teams to work together more efficiently, freeing up precious time for overworked nurses. Despite having proven results, he was let go because the consultants couldn’t fit his already-implemented, already-proven solution into their model. He has now founded a business to sell that same method to health systems as a SaaS business. Traditional consulting firms also worsen a key challenge in healthcare: time pressure. Most health systems plan year-to-year based on government reimbursements. With revenue cycles already complex, consultants often default to short-term cost cutting—an easier sell than long-term change. The result? Innovation stalls, patient experience suffers, and the cycle repeats. If it’s so difficult, why not just leave healthcare alone? Because clearly, patients want better services. And by and large, those closest to the patient aren’t the problem. There is an abundance of clinical excellence in the United States but this doesn’t always translate to the best outcomes or patient experiences. The disconnect lies in how we approach system-level change. While working with a leading cancer center, my team found a big pain point for doctors: low compliance—in other words patients weren’t following instructions. Research revealed that while treatment plans (housed in large binders) were technically sound, they weren’t tailored to patients. As a result, patients would “underperform.” We found that clearer communication, organized around actionable items and digestible content, could drive meaningful improvement. This “user experience–first” investigation, which centered on the needs of both doctors (frustrated by low compliance) and patients (overwhelmed by information), is rarely prioritized in traditional consulting models but is core to a more modern, design-led approach. The house renovation problem Imagine you’re renovating a Victorian mansion with a funky layout. The big consulting approach would be to tell the construction team to spend the allotted budget on turning the largest bedroom into two bedrooms, thereby increasing the home value. Maybe they’d advise a fresh coat of light grey paint, chosen to be least likely to offend potential buyers. But what if the person buying the home doesn’t have people to fill those bedrooms? What if they would be happier with a bolder color? What if in the process of splitting the bedroom, the floorboards are found to have mold? Well, the suit-clad consultants are already gone. You’re on your own, kid. Now imagine a design-led approach. In this scenario, the firm leading strategy is also the one implementing the changes. They spend the budget shifting the plumbing, dealing with mold issues as they arise. They don’t add another bedroom because it’s not needed, even if it would theoretically increase value. They try out a few paint swatches and see market appetite for bolder colors. Buyers are happier—they’re willing to pay more! Everyone wins. From slide decks to solutions Apply this rubric to healthcare. A design-led approach can balance strategic and business goals with the realities of user experience and complexities of implementation. Consul

The healthcare industry has many ills. The payer-provider disconnect creates confusion, limits access, and exacerbates inefficiencies. Doctor and nurse burnout has led to widespread staffing shortages. This is compounded by aging infrastructure, outdated regulation, fragmented care delivery, and overly-complicated legacy systems. The list goes on. But there is a particular cancer that we could eliminate tomorrow: big consulting firms.
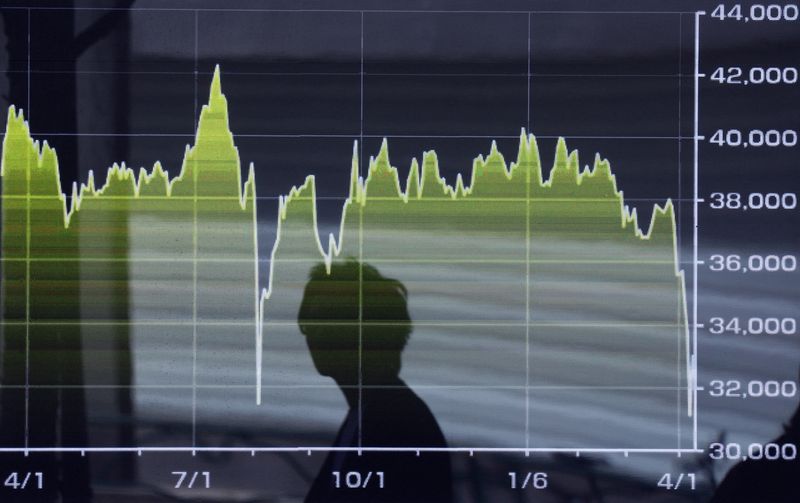
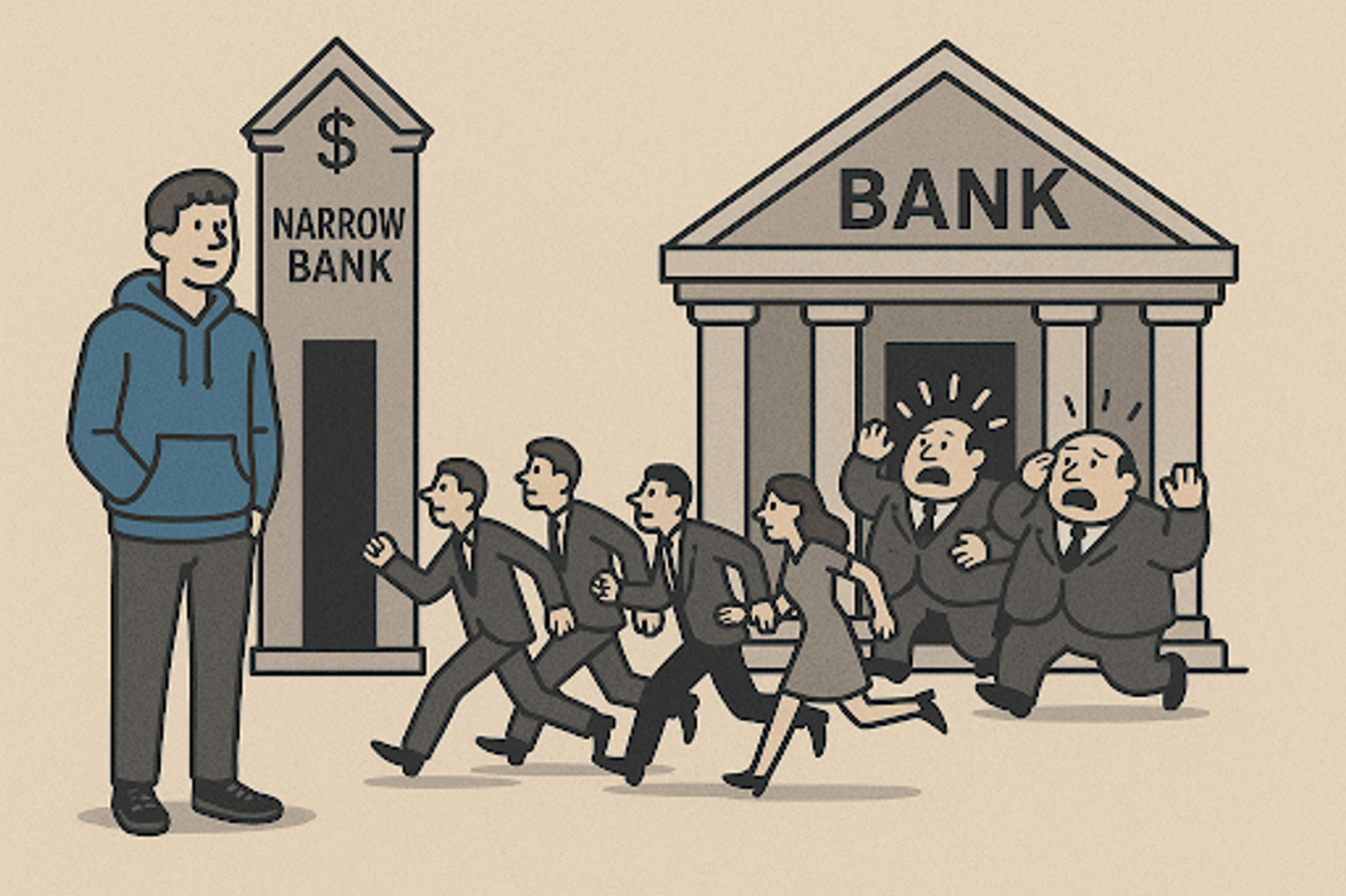
Every year, American healthcare systems spend hundreds of millions of dollars on consulting firms that deliver PDFs instead of solutions. While patients suffer and clinicians burn out, these legacy firms collect their checks and move on—leaving implementation challenges to healthcare institutions they’ve diagnosed but failed to treat.
Proponents of the “Big Five” consulting model would argue that sclerotic institutions need an untainted outsider to parachute in. Someone who isn’t married to the nuances of an existing system. But theorizing is easy to do when you’re not tethered to the results. In healthcare, it’s not just financial results the consultants are off the hook for, it’s people’s lives.
What do providers get with a legacy consulting firm? Well, a sizable stack of documents. With massive fees to match. While a 300-page PDF may impress at first blush, it won’t lead to actionable, sustainable solutions. It certainly won’t allow the health system to rapidly test and refine new models of care delivery, proving which ideas do and don’t work in practice.
Time pressure and fitting solutions in boxes
At Cactus, the design firm I cofounded, one of our clients was let go from a major health system as part of a big consulting cost-cutting round. He had been working to reduce staffing shortages and developed a novel method for care teams to work together more efficiently, freeing up precious time for overworked nurses. Despite having proven results, he was let go because the consultants couldn’t fit his already-implemented, already-proven solution into their model. He has now founded a business to sell that same method to health systems as a SaaS business.
Traditional consulting firms also worsen a key challenge in healthcare: time pressure. Most health systems plan year-to-year based on government reimbursements. With revenue cycles already complex, consultants often default to short-term cost cutting—an easier sell than long-term change. The result? Innovation stalls, patient experience suffers, and the cycle repeats.
If it’s so difficult, why not just leave healthcare alone?
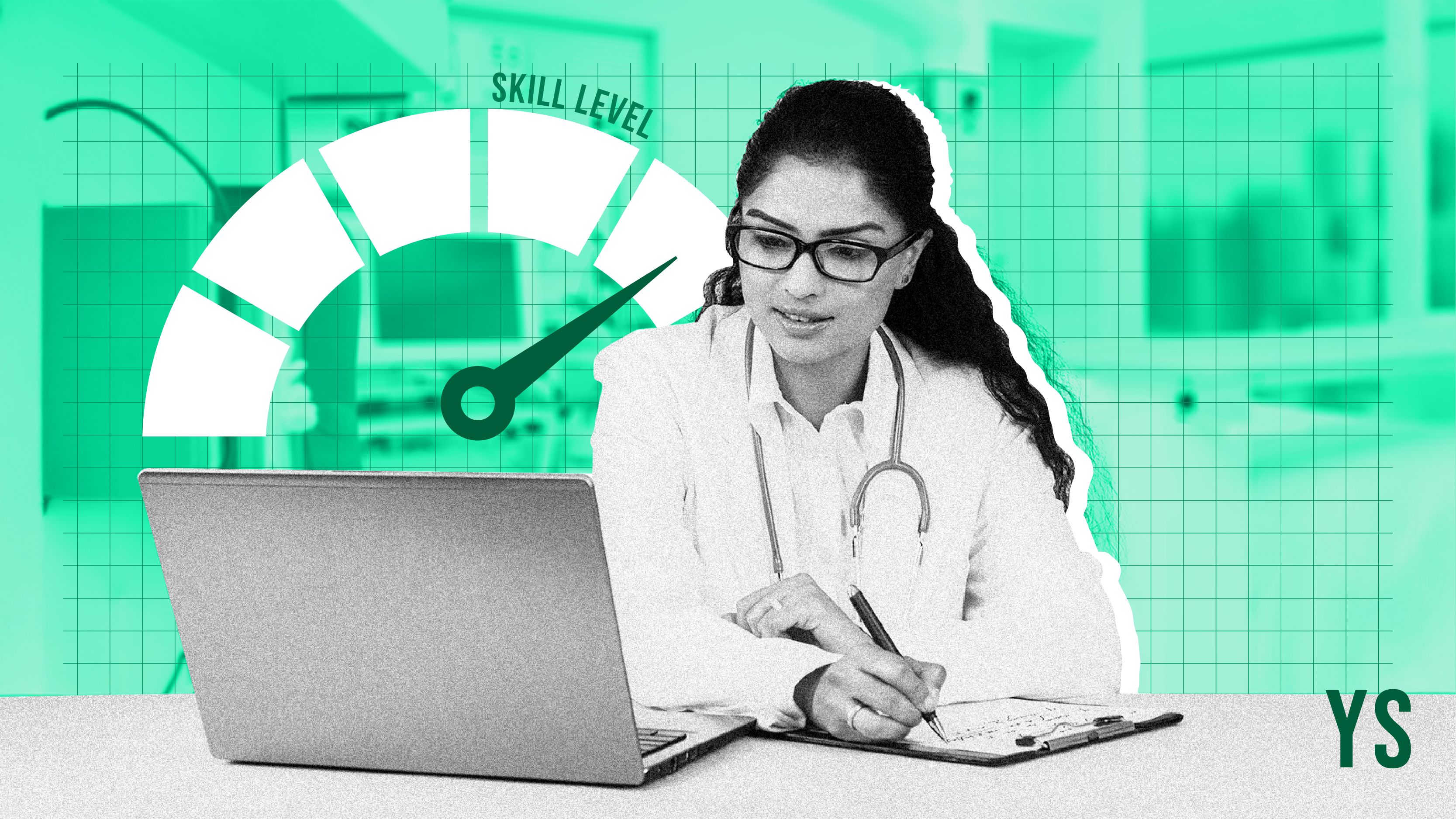
Because clearly, patients want better services. And by and large, those closest to the patient aren’t the problem. There is an abundance of clinical excellence in the United States but this doesn’t always translate to the best outcomes or patient experiences. The disconnect lies in how we approach system-level change.
While working with a leading cancer center, my team found a big pain point for doctors: low compliance—in other words patients weren’t following instructions. Research revealed that while treatment plans (housed in large binders) were technically sound, they weren’t tailored to patients. As a result, patients would “underperform.” We found that clearer communication, organized around actionable items and digestible content, could drive meaningful improvement. This “user experience–first” investigation, which centered on the needs of both doctors (frustrated by low compliance) and patients (overwhelmed by information), is rarely prioritized in traditional consulting models but is core to a more modern, design-led approach.
The house renovation problem
Imagine you’re renovating a Victorian mansion with a funky layout. The big consulting approach would be to tell the construction team to spend the allotted budget on turning the largest bedroom into two bedrooms, thereby increasing the home value. Maybe they’d advise a fresh coat of light grey paint, chosen to be least likely to offend potential buyers. But what if the person buying the home doesn’t have people to fill those bedrooms? What if they would be happier with a bolder color? What if in the process of splitting the bedroom, the floorboards are found to have mold? Well, the suit-clad consultants are already gone. You’re on your own, kid.
Now imagine a design-led approach. In this scenario, the firm leading strategy is also the one implementing the changes. They spend the budget shifting the plumbing, dealing with mold issues as they arise. They don’t add another bedroom because it’s not needed, even if it would theoretically increase value. They try out a few paint swatches and see market appetite for bolder colors. Buyers are happier—they’re willing to pay more! Everyone wins.
From slide decks to solutions
Apply this rubric to healthcare. A design-led approach can balance strategic and business goals with the realities of user experience and complexities of implementation. Consultants that also build can pilot innovations faster, see results faster, reducing overall risk and cost. This type of team can rapidly experiment and improve in a virtuous cycle like the best startups do.
Design-led consulting firms that implement their own changes also have a higher stake in outcomes. They create working prototypes before prescribing final solutions. They iterate based on real-world feedback. This way mistakes are found fast and plans are adjusted before scaling, saving cost and allowing faster and more thorough implementation.
A call to healthcare leaders
To healthcare leaders, I ask: What could you ship in the next 90 days with a design-led approach? What might still be sitting in a binder three years from now with traditional consulting? If the answer is something that could change people’s lives, and I suspect it is, it might be time to ditch the big guys.
Design-led firms offer a fundamentally different relationship: partners who share your risk, commit to real-world results, and aren’t afraid to get their hands dirty implementing solutions. They bring technical talent alongside strategic thinking. They work in weeks, not quarters. Most importantly, they are judged by what they build, not what they recommend.
The question isn’t whether you can afford this approach. The question is whether you can afford not to try it. Because while big consulting firms continue collecting their checks for delivering their slide decks, your patients and workforce are waiting for something better. They deserve it. And with the right partners, you can finally deliver it.
Noah Waxman is CEO and cofounder at Cactus.



![How Social Platforms Measure Video Views [Infographic]](https://imgproxy.divecdn.com/AncxHXS242CT-kDlEkGZi7uQ2k70-ebTAh7Lm14QKb8/g:ce/rs:fit:770:435/Z3M6Ly9kaXZlc2l0ZS1zdG9yYWdlL2RpdmVpbWFnZS9ob3dfcGxhdGZvcm1zX21lYXN1cmVfdmlld3MucG5n.webp)