Menopause is having a “moment”
For many generations, menopause was a taboo topic. Despite 6,000 women reaching menopause in the U.S. each day, this pivotal stage in a woman’s life has been sidelined and neglected in the broader healthcare landscape. While symptoms can be debilitating for many women, a lack of research and medical training on menopause often results in these issues being misdiagnosed or dismissed. Unfortunately, this can translate to reduced insurance coverage and higher out-of-pocket costs for millions of women trying to manage their symptoms through prescribed medications and treatments. Today, the tide is turning on menopause, due in part to celebrities including Oprah, Halle Berry, and Drew Barrymore speaking publicly about their experiences. They are advocating for greater resources for women, and there is increased acceptance among the current generation in discussing menopause openly. A growing number of startups, like Elektra Health and Midi Health, are offering women more education, access to care, and a virtual community to help them face their menopause journeys. Even legislators are taking note, proposing changes to improve affordability and increase education for medical professionals across several states. But there’s much more to be done, especially when it comes to education and affordability. Last month, our GoodRx team released findings from a new survey exploring the financial difficulties women face when navigating menopause. The data illustrated a greater need to address access and affordability gaps in menopause care, and underscored the importance of evolving our healthcare system to support women at every stage of life. Affordability challenges in menopause care Even as the conversation around menopause grows, women are routinely priced out of the treatments they need to manage their symptoms. Our survey, conducted in February 2025, found that 21% of women have put off or avoided menopause treatment due to financial concerns. And 12% reported having to make financial trade-offs, such as cutting back on other essential expenses, just to afford their care. It’s not surprising that women are struggling to afford menopause care, as list prices for menopause medications have risen almost 60% over the last decade, and these costs trickle down to the consumer. Unfortunately, insurance coverage isn’t always a reliable solution. Only 26% of women have their menopause-related prescriptions fully covered by insurance, and 8% don’t have their prescriptions covered at all. The link is clear: Lower costs are crucial in helping more women access the menopause care they need. Improve the care gap in menopause Beyond cost itself, there is an unmet need to improve access to menopause care. The issue starts in medical schools, where most programs offer limited education on perimenopause, menopause, and post-menopause. As a result, the majority of primary care physicians don’t have the skillset needed to help their patients manage symptoms. Even within OB-GYN training programs, research shows that less than a third of residency programs have any type of menopause curriculum. When unable to get answers from their usual physicians, many women turn to certified menopause specialists to seek help with their symptoms. But, as of now, there is only one menopause-certified specialist available for every 30,000 menopausal women in the U.S. By improving the full spectrum of menopause care and making sure every primary care physician and OB-GYN has the training they need, we can help break down access barriers and help more women address their symptoms. Unlock new frontiers in menopause care With healthcare industry leaders understanding the need to better support women transitioning into menopause, promising new treatments are emerging. For example, elinzanetant is currently in late-stage clinical development to address hot flashes associated with menopause—one of the most common symptoms. As new medications continue to undergo trials and enter the market, ensuring widespread availability is crucial. By better addressing hot flashes, women can improve their quality of life during menopause. This doesn’t just benefit individuals, but improves the healthcare sector as a whole. A more supportive future for women There’s no silver bullet that can help lower costs and make menopause treatments more accessible. For healthcare leaders, menopause’s growing economic burden is not just a health concern, but a call for systemic change. There are several levers we can pull to create a better, more supportive system for women. First, manufacturers of the most effective treatments for menopause, like menopausal hormone therapy, can look beyond insurance coverage and find ways to support women who are forced to pay out of pocket for these medications. While copay cards can be incredibly helpful for many high-cost prescriptions, these types of discount programs have low awarenes
For many generations, menopause was a taboo topic. Despite 6,000 women reaching menopause in the U.S. each day, this pivotal stage in a woman’s life has been sidelined and neglected in the broader healthcare landscape. While symptoms can be debilitating for many women, a lack of research and medical training on menopause often results in these issues being misdiagnosed or dismissed. Unfortunately, this can translate to reduced insurance coverage and higher out-of-pocket costs for millions of women trying to manage their symptoms through prescribed medications and treatments.
Today, the tide is turning on menopause, due in part to celebrities including Oprah, Halle Berry, and Drew Barrymore speaking publicly about their experiences. They are advocating for greater resources for women, and there is increased acceptance among the current generation in discussing menopause openly. A growing number of startups, like Elektra Health and Midi Health, are offering women more education, access to care, and a virtual community to help them face their menopause journeys. Even legislators are taking note, proposing changes to improve affordability and increase education for medical professionals across several states.
But there’s much more to be done, especially when it comes to education and affordability. Last month, our GoodRx team released findings from a new survey exploring the financial difficulties women face when navigating menopause. The data illustrated a greater need to address access and affordability gaps in menopause care, and underscored the importance of evolving our healthcare system to support women at every stage of life.
Affordability challenges in menopause care
Even as the conversation around menopause grows, women are routinely priced out of the treatments they need to manage their symptoms. Our survey, conducted in February 2025, found that 21% of women have put off or avoided menopause treatment due to financial concerns. And 12% reported having to make financial trade-offs, such as cutting back on other essential expenses, just to afford their care.
It’s not surprising that women are struggling to afford menopause care, as list prices for menopause medications have risen almost 60% over the last decade, and these costs trickle down to the consumer. Unfortunately, insurance coverage isn’t always a reliable solution. Only 26% of women have their menopause-related prescriptions fully covered by insurance, and 8% don’t have their prescriptions covered at all. The link is clear: Lower costs are crucial in helping more women access the menopause care they need.
Improve the care gap in menopause
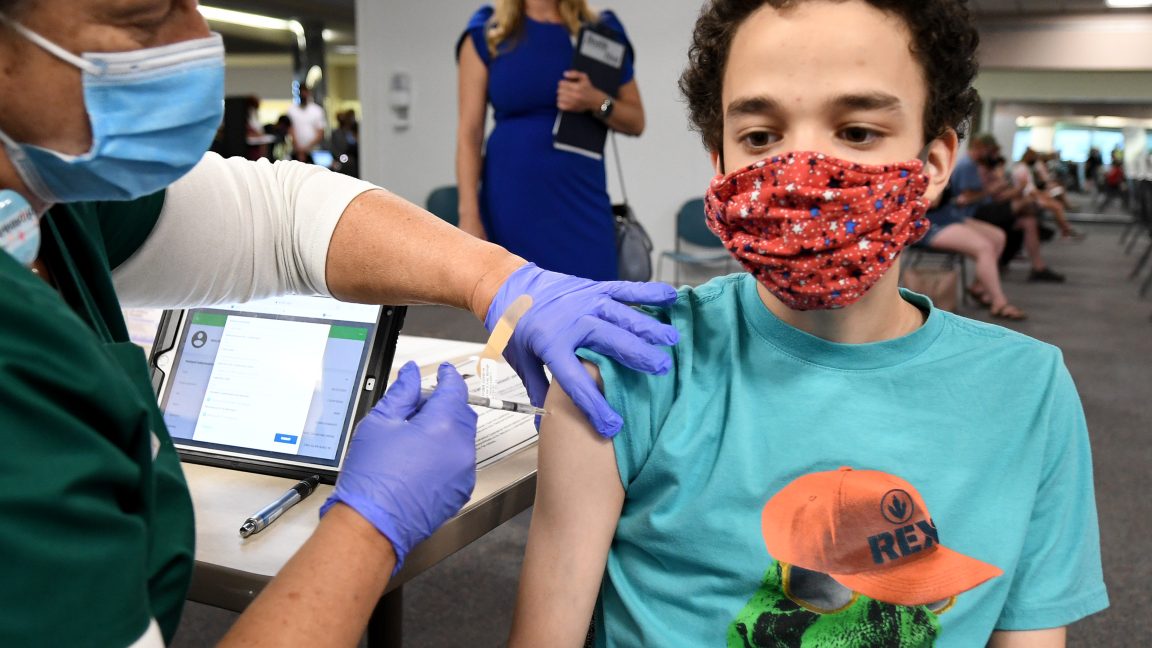
Beyond cost itself, there is an unmet need to improve access to menopause care. The issue starts in medical schools, where most programs offer limited education on perimenopause, menopause, and post-menopause. As a result, the majority of primary care physicians don’t have the skillset needed to help their patients manage symptoms. Even within OB-GYN training programs, research shows that less than a third of residency programs have any type of menopause curriculum.
When unable to get answers from their usual physicians, many women turn to certified menopause specialists to seek help with their symptoms. But, as of now, there is only one menopause-certified specialist available for every 30,000 menopausal women in the U.S. By improving the full spectrum of menopause care and making sure every primary care physician and OB-GYN has the training they need, we can help break down access barriers and help more women address their symptoms.
Unlock new frontiers in menopause care
With healthcare industry leaders understanding the need to better support women transitioning into menopause, promising new treatments are emerging. For example, elinzanetant is currently in late-stage clinical development to address hot flashes associated with menopause—one of the most common symptoms.
As new medications continue to undergo trials and enter the market, ensuring widespread availability is crucial. By better addressing hot flashes, women can improve their quality of life during menopause. This doesn’t just benefit individuals, but improves the healthcare sector as a whole.
A more supportive future for women
There’s no silver bullet that can help lower costs and make menopause treatments more accessible. For healthcare leaders, menopause’s growing economic burden is not just a health concern, but a call for systemic change. There are several levers we can pull to create a better, more supportive system for women.
First, manufacturers of the most effective treatments for menopause, like menopausal hormone therapy, can look beyond insurance coverage and find ways to support women who are forced to pay out of pocket for these medications. While copay cards can be incredibly helpful for many high-cost prescriptions, these types of discount programs have low awareness. Pharmaceutical manufacturers can turn to trusted consumer resources, like GoodRx, to offer exclusive patient pay programs for those without adequate coverage on these medications. We launched this exact type of partnership with Pfizer’s portfolio of menopause hormone therapies last year and are seeing high uptake. We can further broaden access by working with other manufacturers in this space.
Of course we still need to evolve our existing health insurance benefit structures to ensure they adequately support the diverse needs of women going through menopause. This includes providing comprehensive coverage for hormone replacement therapies and other menopausal treatments without prohibitive costs. Employers play a role here, too, and can advocate for health plans that respect women’s specific medical needs, which can in turn improve overall job satisfaction, productivity, and tenure.
As both a leader and a woman navigating these same healthcare challenges, I’m optimistic about the future. By making menopause management easier, we not only enhance the quality of life for individual women, but generate positive impacts on families and the larger healthcare system.
Dorothy Gemmell is chief commercial officer and president, manufacturer solutions at GoodRx.